Metastatic Melanoma: A Deep Dive into the Aggressive Form of Skin Cancer

Melanoma, a type of skin cancer, can be a frightening diagnosis. But within the spectrum of melanoma, metastatic melanoma stands out as particularly aggressive and challenging to treat. In this article, we’ll explore what sets metastatic melanoma apart, its seriousness, conventional treatment approaches, the promising role of immunotherapy, and the intriguing connection with dendritic cell dysfunction.
Background
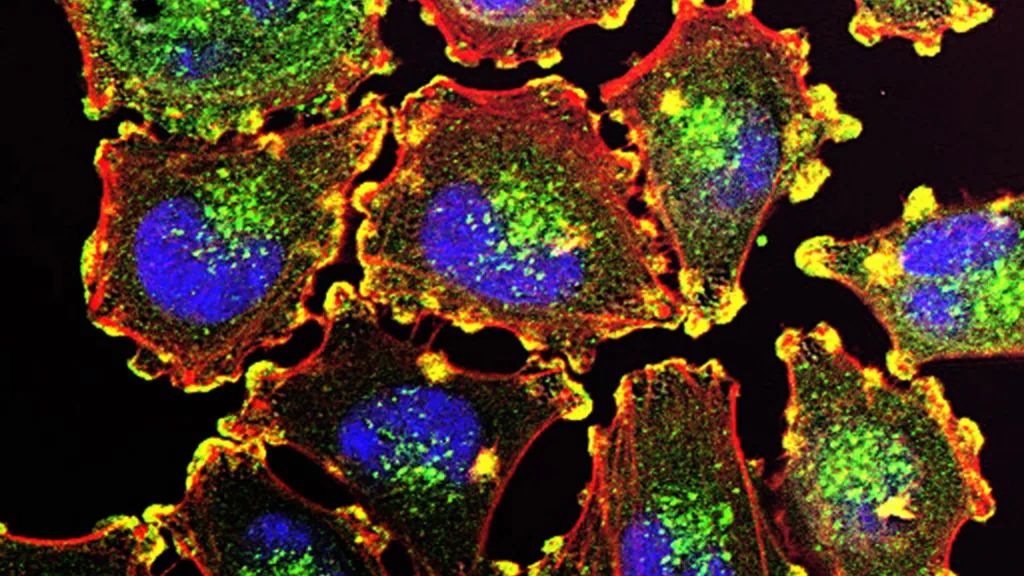
Melanoma arises from melanocytes, the cells responsible for producing melanin, the pigment that gives skin its color. When melanocytes begin to grow out of control, they can form malignant tumors, leading to melanoma. While early-stage melanomas are often treatable with surgery, metastatic melanoma is a different story altogether.
The common misconception that melanoma is solely a surface-level skin cancer overlooks the fact that melanoma can indeed originate within the body, not just on the skin. While cutaneous melanoma, which develops from melanocytes in the skin, is the most well-known type, melanoma can also arise in other parts of the body where melanocytes are present or migrate to during fetal development. This includes mucosal surfaces, the eyes, and even within internal organs.
- Cutaneous Melanoma: This is the most prevalent form of melanoma and originates from melanocytes in the skin. Cutaneous melanomas typically appear on sun-exposed areas like the face, neck, arms, and legs, but they can develop anywhere on the body, including areas not exposed to sunlight.
- Mucosal Melanoma: Melanocytes are also found in mucosal membranes lining various internal organs, such as the mouth, nasal passages, throat, digestive tract, urinary tract, and genital areas. Mucosal melanoma can develop in these tissues and often presents as a dark, irregularly shaped lesion. Mucosal melanomas are relatively rare but tend to be diagnosed at a more advanced stage due to their hidden location.
- Ocular Melanoma: Melanocytes are present in the eyes, particularly in the uvea, which is the middle layer of the eye. Ocular melanoma, also known as uveal melanoma, originates from melanocytes within the eye and can affect structures such as the iris, ciliary body, or choroid. Unlike cutaneous melanoma, ocular melanoma may not be readily visible and can be detected during routine eye exams.
- Internal Organ Melanoma: Although less common, melanoma can develop within internal organs such as the lungs, intestines, or brain. These cases often arise from melanocytes that have migrated during embryonic development and can present unique challenges in diagnosis and treatment.
The ability of melanoma to arise from sites beyond the skin underscores the importance of vigilance in detecting and diagnosing this disease. Patients and healthcare providers should be aware of the potential for melanoma to manifest internally, especially in individuals with risk factors such as a history of extensive sun exposure, family history of melanoma, or presence of atypical moles.
Moreover, the treatment and prognosis of melanoma can vary depending on its location and stage at diagnosis. While cutaneous melanoma is more commonly treated with surgical excision, mucosal, ocular, and internal organ melanomas may require a multidisciplinary approach involving surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy.
Understanding Metastatic Melanoma:
Metastatic melanoma, also known as stage IV melanoma, is characterized by cancer cells spreading from the primary site (usually the skin) to distant organs like the lungs, liver, brain, or bones. This metastatic spread makes treatment significantly more challenging and reduces the likelihood of successful outcomes.
Metastatic melanoma is one of the most aggressive forms of skin cancer, with a notoriously poor prognosis if left untreated. It can quickly become life-threatening due to its ability to invade vital organs and resist traditional therapies.
Without treatment, the average survival time for patients with stage IV metastatic melanoma is often measured in months. However, with the advent of newer therapies, such as immunotherapy and targeted therapy, some patients have experienced prolonged survival, with a subset achieving long-term remission.
Despite advancements in treatment, not all patients respond favorably to therapy, and disease progression remains a significant concern. Some patients may develop resistance to treatment over time, leading to disease recurrence or metastasis.
Conventional Treatment Approaches:
Historically, treatment options for metastatic melanoma were limited, often relying on chemotherapy, surgery, or radiation therapy, which had limited effectiveness and significant side effects. However, advancements in medical research have led to the development of targeted therapies and immunotherapies, revolutionizing the treatment landscape for this disease.
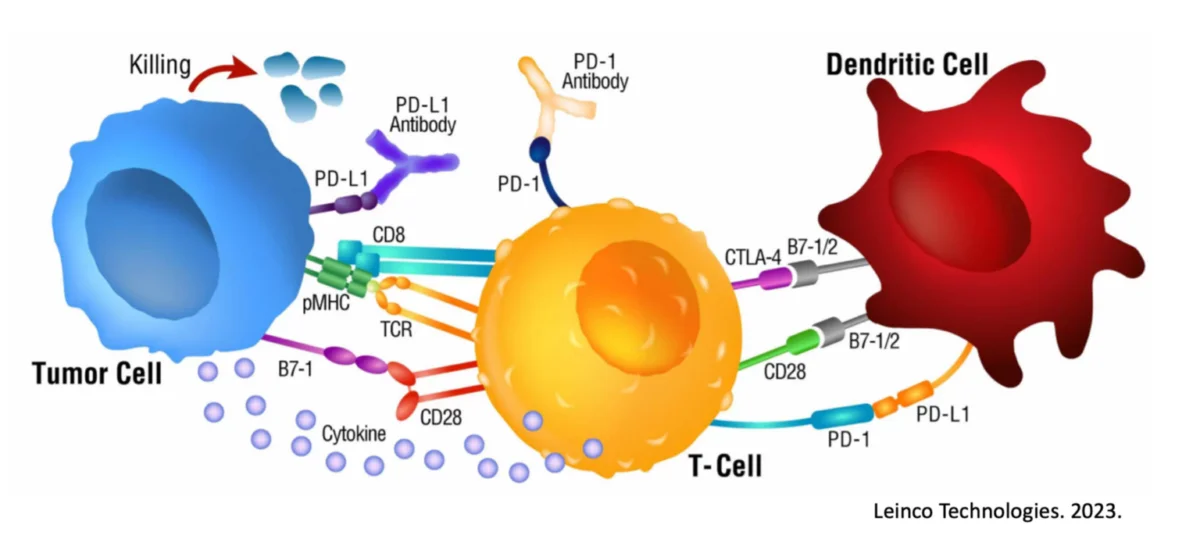
Immunotherapy has emerged as a game-changer in the management of metastatic melanoma. By harnessing the power of the body’s immune system to recognize and destroy cancer cells, immunotherapies such as checkpoint inhibitors (e.g., pembrolizumab, ipilimumab) and adoptive cell therapy have shown remarkable efficacy in extending survival and inducing durable responses in some patients.

Dendritic Cell Dysfunction:
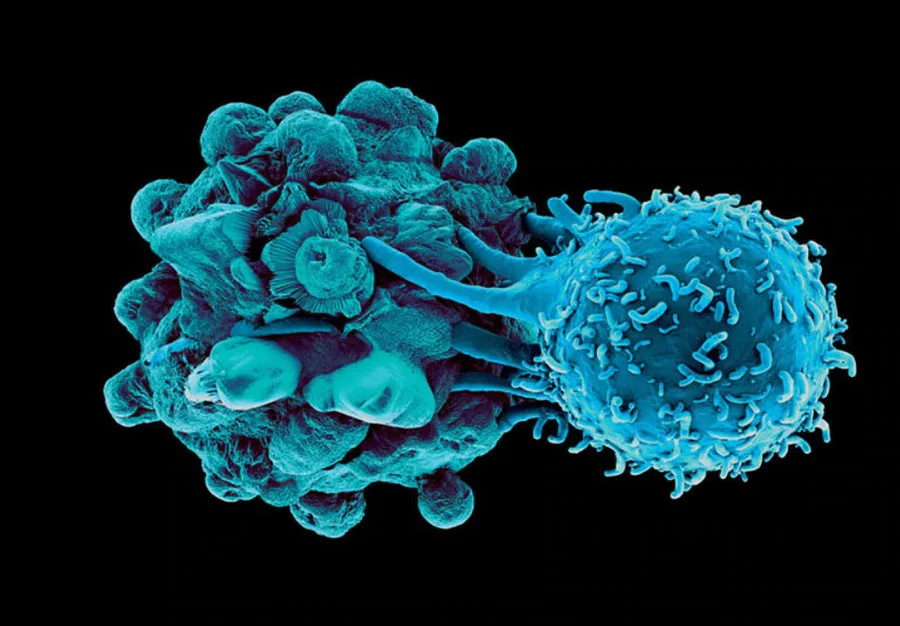
Dendritic cells play a crucial role in initiating and regulating immune responses, including the recognition of cancer cells as foreign invaders. However, in metastatic melanoma, dysfunction of dendritic cells has been observed, impairing their ability to effectively prime T cells and mount an anti-tumor immune response.
Recent studies have shed light on the mechanisms underlying dendritic cell dysfunction in melanoma, including alterations in signaling pathways, immunosuppressive microenvironments within tumors, and interactions with tumor cells and other immune cells.
Understanding and addressing dendritic cell dysfunction may hold the key to enhancing the effectiveness of immunotherapy and overcoming resistance mechanisms in metastatic melanoma. Strategies aimed at restoring dendritic cell function or targeting alternative pathways involved in tumor immune evasion are currently being investigated in preclinical and clinical studies, offering hope for improved outcomes for patients with this challenging disease.
In a recent study, strong Dendritic Cell metabolic profiles were linked to positive outcomes when dealing with metastatic melanoma. Essentially, the more immunostimulatory the Dendritic Cell, the better the odds of remission. Additionally, it has been shown that Dendritic Cell vaccines are able to provide a wide breadth of melanoma antigen targeting to the effector immune cells responsible for targeting and destroying this cancer. This makes it infinitely more difficult for the cancer to be hidden post a vaccine like this, and the immune system finally has an edge. Mathematical models have outlined how a Dendritic Cell vaccine plus checkpoint inhibitor can effectively eradicate tumor cells, a feat witnessed on multiple occasions with Immunocine.
Taken together, there is reason for optimism when combining the unique robustness and durable immunological memory generated from the Immunocine Dendritic Cell platform with what many have witnessed in general regarding Dendritic Cells and metastatic melanoma. The scientific rationale plus Immunocine’s own exciting results in this cancer further elevate this personalized therapy as a legitimate weapon in overcoming this assiduous cancer.
READ THIS NEXT
Team Spotlight: Dr. Elideth Angulo, MD
A compassionate and dedicated healthcare professional, Dr. Elideth Angulo’s journey in medicine began with a childhood dream. Originally f
Read MoreUnlocking Better Cancer Treatment Results with Exercise
Babette, now cancer-free after her treatment at Immunocine, discovered both peace of mind and health benefits through daily walks with her d
Read MoreOn Air with Immunocine: Matt Halpert Joins Haylie Pomroy to Discuss the Future of Cancer Treatment
Listen to this Episode on Apple Podcasts Listen to this Episode on Spotify In this episode of the Hope and Help for Fatigue and Chronic Illn
Read More