Cancer Cells Hiding in Other Cancer Cells?
As we outlined in our post dedicated to Head & Neck Cancer, the Immune System has the inherent ability to find and destroy cancer cells. In fact, it does this for you every day! Since humans already have this natural ability, scientists are continually researching why cancer cells are able to avoid detection and ultimately grow into tumors.
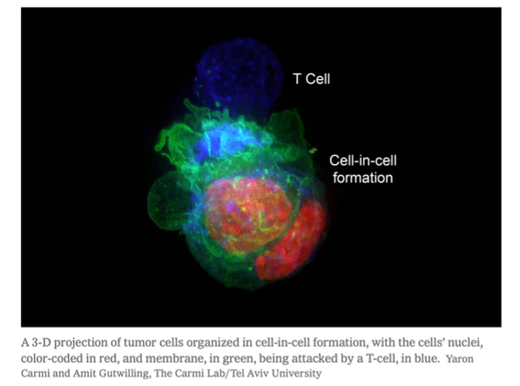
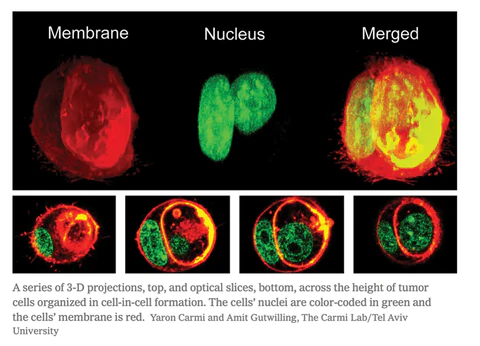
Recently, scientists have discovered a new way that cancers are able to avoid detection: hiding in other cancer cells. This mechanism not only allows the cancer cells to hide, but it actually creates a protective shell around the inner cancer cell, which increases resistance to immune responses and most cancer treatments.1
Fortunately, this does not hinder all cancer treatments. Cancer treatments, such as Immunocine’s Treatment, can generate Immunological Memory and be able to overcome this newly discovered form of hiding. Let’s dive in!
The Impact on Various Cancer Treatments
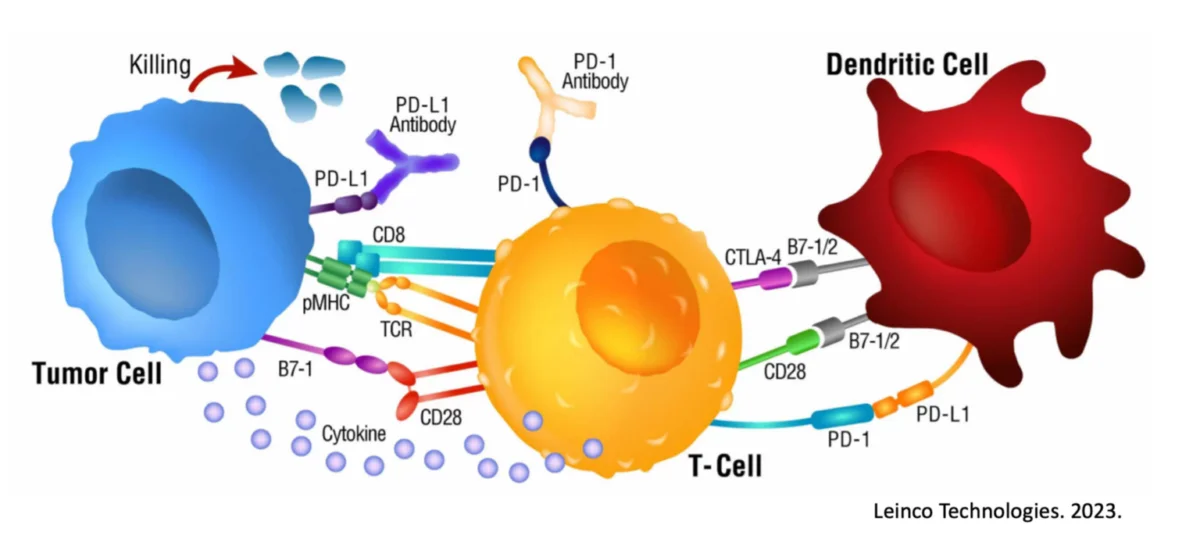
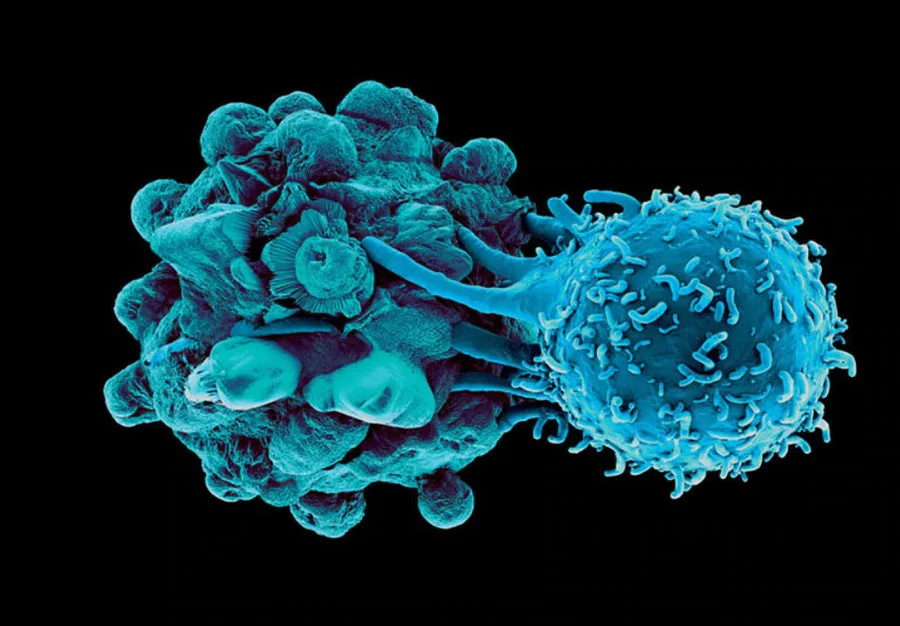
Immunotherapies generally aim to activate a special group of cells known as killer T-cells, which are responsible for the immune attack against the spreading cancer2. These cells can identify cancer cells and destroy them once in contact3, 4. However, this is not always 100% effective, which is often the result of cancer cells being naturally good at avoiding detection by the Immune System. This includes examples such as gene mutation to develop resistance and/or activating immunosuppressive signals5,6,7.
To further understand how cancers react to various forms of Immunotherapy, the researchers of this latest publication developed several models in which resistant tumors would relapse following various Immunotherapy treatments.
In both mice and humans, they found that the tumor cells remaining after Immunotherapy treatments could form ‘cell-in-cell’ structures that were actually impenetrable. While the outer cells in this formation are often killed by the Killer T cells, the inner cells survived for weeks.
Senior author Yaron Carmi Ph.D. stated that seeing the cancer hiding for weeks to months was like “seeing the devil8.”
As most forms of cancer treatment are provided over a specific period of time, this waiting would render these treatments ineffective. Once the treatment, whether it be Chemotherapy or a Checkpoint Inhibitor regimen is complete, the hiding cancer cells could emerge and continue to wreak havoc.
The Importance of Immunological Memory
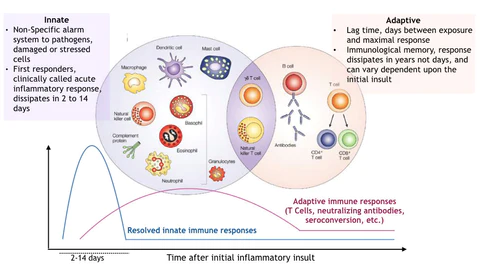
Our bodies already have a solution to this waiting game. As part of a natural immune response, our bodies develop Immunological Memory against the threat. This Immunological Memory allows our body to fight off the pathogen more effectively the next time we encounter that specific threat.
Whether it takes weeks or months, research has shown that these cancer cells will eventually come out of hiding. This does no good if the specific cancer treatment has stopped. However, if the Immune System has developed this Immunological Memory, it will be ready to attack when presented with the chance.
Fortunately for Immunocine patients, Immunological Memory is quite probable with our treatment. It is this Immunological Memory that allows our treatment to continue to keep fighting a patient’s cancer long after they have gone home.
Generating Immunological Memory Against Cancer Cells
Why is Immunocine able to generate Immunological Memory when so many other treatments fail to do so? The simple answer is that the Immunocine Treatment creates a complete and natural immune response against the patient’s cancer (Source). Instead of short cutting the Immune System with genetically modified CAR-T cells or simply providing a medication like a Checkpoint Inhibitor, Immunocine starts at the top of the Immune Response: the Dendritic Cell.
In a study conducted in 2016, our Immunotherapy Protocol was tested against a popular Chemotherapy drug in regard to relapse and Immunological Memory.9
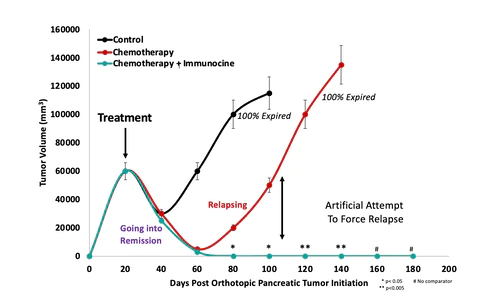
The mice that received our Immunotherapy would not relapse despite attempts to give them the same form of Pancreatic Cancer that they had been treated with. The mice only receiving Chemotherapy quickly relapsed and ultimately perished.
As the general of the Immune System, the Dendritic Cell does so much more than simply attacking the cancer. It activates the Immune System to search the entire body for cancer cells, to target all variations of the mutated cancer cells, and to develop Immunological Memory against future growth of the cancer. This process is no different than what our bodies do when stopping a viral infection.10,11,12
Additional Advantages of Immunocine’s Treatment
As part of the Immunocine protocol, a patient’s cancer cells are taken to the lab where they are deconstructed to its base components, including:
All of the messenger RNA – which encodes 100% of the instructions to form the cancer from the inside
The entire protein expression library – which functions on and within every structure inherent to the cancer cells.
Therefore, it is irrelevant to us whether the cancer cells began as stand-alone cells, in clusters, or in ‘cell-in-cell’ architecture because all of these components are used for the patient’s personalized treatment.
In summary, the Immunocine Dendritic Cell Treatment is not a drug with a defined half-life, but rather is a “living therapy” capable of self-propagation and proliferation. It is able to continue until the cancer threat is eliminated and is able to activate again if the same cancer cells emerge at a later time.
References
As a note, any publication that is bolded is a publication specifically in reference to Immunocine’s Immunotherapy.
Gutwillig, A. et al. Transient cell-in-cell formation underlies tumor relapse and resistance to immunotherapy. Elife 11 (2022).
Waldman, A.D., Fritz, J.M. & Lenardo, M.J. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol 20, 651-668 (2020).
Cullen, S.P., Brunet, M. & Martin, S.J. Granzymes in cancer and immunity. Cell Death Differ 17, 616-623 (2010).
Hurkmans, D.P. et al. Granzyme B is correlated with clinical outcome after PD-1 blockade in patients with stage IV non-small-cell lung cancer. J Immunother Cancer 8 (2020).
Khong, H.T. & Restifo, N.P. Natural selection of tumor variants in the generation of “tumor escape” phenotypes. Nat Immunol 3, 999-1005 (2002).
Cornel, A.M., Mimpen, I.L. & Nierkens, S. MHC Class I Downregulation in Cancer: Underlying Mechanisms and Potential Targets for Cancer Immunotherapy. Cancers (Basel) 12 (2020).
Jiang, X. et al. Role of the tumor microenvironment in PD-L1/PD-1-mediated tumor immune escape. Mol Cancer 18, 10 (2019)
Kolata, G. A Devious Cellular Trick Cancers Can Use to Escape Your Immune System. New York Times. 2022 October 4th, 2022; Sect. 3
Vanaja Konduri, Dali Li, Matthew M. Halpert, et al. (2016) Chemo-immunotherapy mediates durable cure of orthotopic KrasG12D/p53−/− pancreatic ductal adenocarcinoma, OncoImmunology, 5:9, e1213933
Halpert, M.M. et al. MHC class I and II peptide homology regulates the cellular immune response. FASEB J 34, 8082-8101 (2020).
Halpert, M.M. et al. Dendritic Cell-Secreted Cytotoxic T-Lymphocyte-Associated Protein-4 Regulates the T-cell Response by Downmodulating Bystander Surface B7. Stem Cells Dev 25, 774-787 (2016).
Decker, W.K. & Shpall, E.J. Progress in dendritic cell immunotherapy: elucidating the enigma of Th-1 polarization. Hum Vaccin 4, 162-164 (2008).
READ THIS NEXT
The Integration of Melatonin in Cancer Immunotherapy: Advancing Cancer Treatment Strategies
Treating late-stage cancers is one of the most persistent and challenging hurdles in contemporary medical practice. Standard treatments—th
Read MoreTeam Spotlight: Dr. Elideth Angulo, MD
A compassionate and dedicated healthcare professional, Dr. Elideth Angulo’s journey in medicine began with a childhood dream. Originally f
Read MoreOvercoming a Rare & Aggressive Kidney Cancer with Immunocine: Justin’s Story
In the prime of his life, Justin was living the life many dream of — raising three young children with his wife and staying in peak physic
Read More