Dr. Nasha Winters’ Mission to Create a New Standard of Cancer Treatment

For decades, Dr. Nasha Winters has been a dynamic force in the field of integrative oncology with an emphasis on the metabolic approach to cancer. Her journey began with a personal battle with cancer at the age of 19 — she received a diagnosis of end-stage ovarian cancer and was given 3 to 6 months to live.
Dr. Winters is on a mission to make integrative oncology a standard, accessible part of healthcare. Across the globe, she explores clinics, scrutinizes protocols and meets with leading experts to help them apply metabolic approaches for patients.
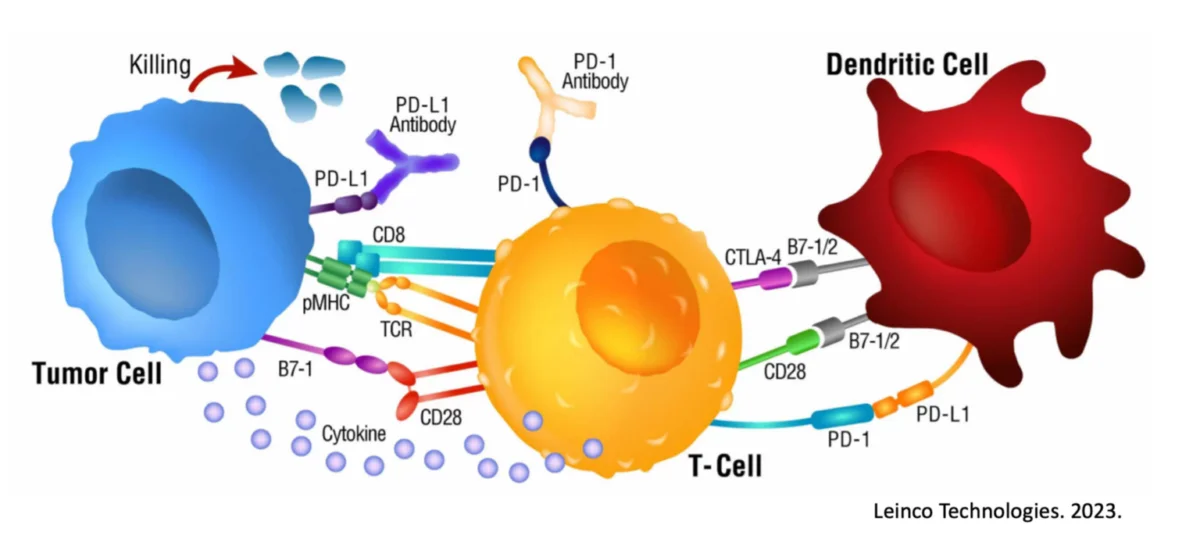
When Dr. Winters was introduced to the dendritic cell treatment that Immunocine had developed, she was initially skeptical — DC therapy historically has led to inconsistent results. But after thorough analysis of the data and patient success stories, she has become a vocal supporter of Immunocine.
We interviewed Dr. Winters to get to know her better, learn more about her approach and discover why she thinks the Immunocine Dendritic Cell Treatment is special.
How would you describe yourself?
Tenacious! High energy, high vision, and high passion that thrives in community and networking and being an ‘agent of change.
Why did you go down the path you’ve chosen?
Cancer was my opportunity to truly live. Honestly, I had been on the fence about that and thanks to some significant traumas in my youth, there were several times where I attempted to take my own life. That all changed when I was met face to face with my mortality at 19 years old. Fast forward—I never wanted to work with cancer, in fact, I wanted as far away from it as possible given what I had been through—however, cancer and those dealing with a cancer diagnosis had other plans for me. Now, I can’t imagine my life without this thing called cancer.
What are your ultimate goals?
To change healthcare in general and cancer care in particular and make integrative oncology standard of care and accessible by all.
Why do you think so often the things you and Immunocine offer patients are not routinely offered by Standard of Care?
How much time do you have to answer this question? LOL.
- We continue to approach cancer the wrong way. It is not a genetic disorder and yet our entire infrastructure to study, evaluate for, and treat cancer is based on this premise.
- There is a lot invested in this outdated/antiquated theory and it is difficult to turn that around when we have now passed the trillion-dollar mark with little or no change in cancer outcomes since war was waged on it in 1971.
- The medical field doesn’t always ask the right questions.
- Though we have come a long way in the way we can Test, Assess, and Address (TM) patients, rarely, if ever, are we applying it in the standard of care environment. So though we might do tissue or blood biopsies, we rarely, if ever start with treating the patients with that information in mind, for example. We continue to follow the assembly line of treatment and don’t offer the more updated versions until the other therapies fail our patients.
- No one wants to fund studies in integrative/alternative therapies, especially when they won’t have the same potential for return on investment. And related, there is a lack of scalability — difficult to scale N of 1 care.
Those are just a few things limiting a more precise, personalized, and modernized approach. Most, if not all ‘alternative’ therapies that support Standard of Care are out of pocket costs which drastically limits who can access a better approach with better outcomes.
What were your previous thoughts on DC therapy?
Historically, since the late 1990’s, I’ve had patients travel to Europe, SE Asia and Mexico to receive DC therapy. I have seen little or no effect as well as terrible progression while receiving these ‘empty treatments’ — so I had all but written it off. I think the (biological) concept was always good, we just hadn’t caught up with our technology until now and I still anticipate it improving for years to come.
What has made you a supporter of Immunocine?
Patients and data. Plain and simple. Though I am an avid researcher and appreciate the data, I also pay attention to what is helping my patients, whether it came through rigorous studies or not. Because I am data driven, I collect the metrics, I review the patient’s experience, and I follow the line of thinking. There is absolutely nothing wrong with bedside to bench research if it is evidence informed while we are simultaneously doing the bench to bedside (which can take an average of 17 years to go through the process of study before it is considered standard of care.
To learn more about Dr. Nasha Winters, visit her website, follow her on Instagram and check out her book “The Metabolic Approach to Cancer.”
READ THIS NEXT
Why Cancer May Stop Responding to Treatment — The Importance of Adaptive Cancer Therapies
Cancer is a complex and challenging disease to treat. While many cancers initially respond well to treatment, it’s not uncommon for th
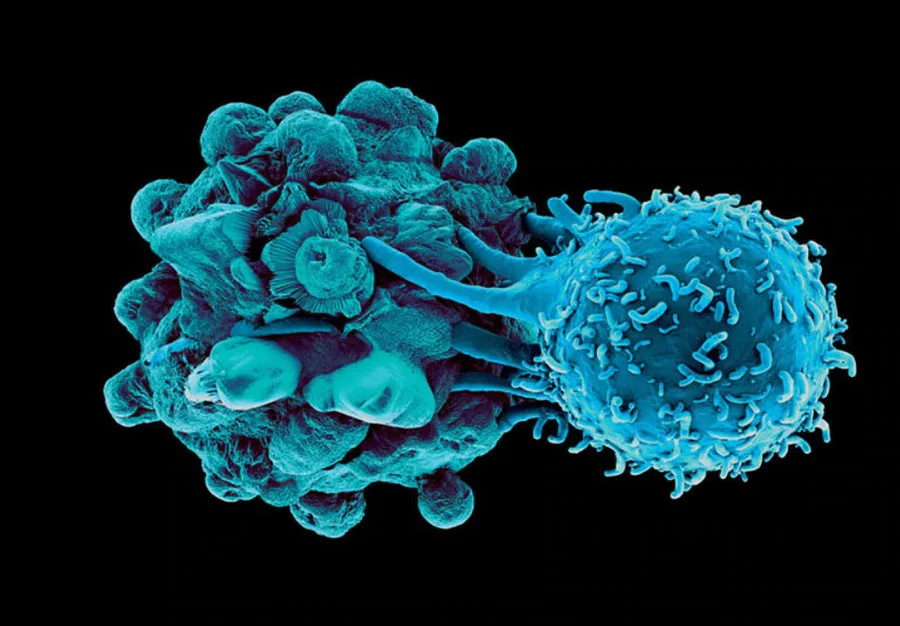
Read MoreThe Unsung Heroes: Dendritic Cells in the Battle Against Pancreatic Cancer
Pancreatic cancer stands as one of the most formidable adversaries in the realm of oncology. This silent killer often evades early detection
Read MoreInflammation in Cancer
In today’s world, chronic inflammation is an ever-present challenge linked to serious diseases, notably cancer. However, the pa
Read More